Concern Over Long-Term Effects of COVID-19 on our Health Care Personnel
Written by Joanne Byron, BS, LPN CCA, CHA, CHCO, CHBS, CHCM, CIFHA, CMDP, OHCC, ICDCT-CM/PCS
March 29, 2021
More...
Article Summary
A New crisis may be emerging which has the ability to dramatically affect our healthcare workers and thus the healthcare industry entirely, it is known as “Brain Fog”. The COVID-19 Pandemic has certainly changed much of our daily life; this of course includes our professional life as well. Furthermore, investigating and understanding the long-term effects of this disease, even in regards to mild cases, has only just begun. This article brings forth insight concerning new research and findings for the consequences of a COVID-19 infection and the ramifications for those working in the healthcare setting.
SARS-CoV-2, more commonly known as the COVID-19 (Coronavirus disease 2019) global pandemic, has disrupted all sectors of society. According to the Centers for Disease Control (CDC) and as demonstrated daily on your local news channel, health care settings in general, and long-term care settings in particular, can be high-risk locations for SARS-CoV-2 exposure and transmission.
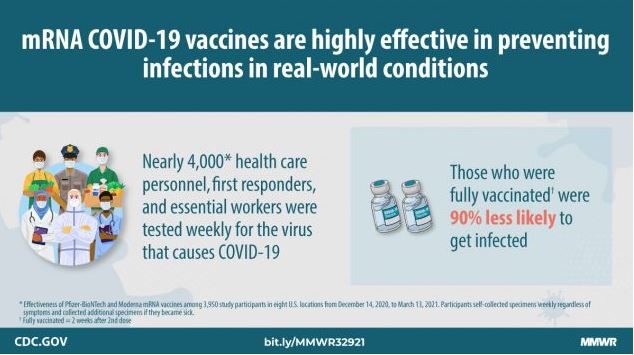
Health care personnel (HCP) are defined as paid and unpaid persons serving in health care settings who have the potential for direct or indirect exposure to patients or infectious materials. According to RegisteredNursing.org, in any given state, 7-26% of coronavirus infections are healthcare workers. Healthcare workers are putting themselves at considerable risk of infection as they work to care for others and many are refusing vaccination.
Scientists are learning more as time passes during this pandemic. We are learning that many organs besides the lungs are affected by COVID-19 and there are many ways the infection can affect someone’s health. “Long Haulers” is a term coined for those with post-COVID-19 syndrome or “long COVID-19”, according to Mayo Clinic, when those infected with even a mild version of the disease continue to experience symptoms or lingering effects.
How COVID-19 Attacks the Brain
Cognitive dysfunction, sometimes called “brain fog” tops the list of neurologic complaints in patients with long-haul COVID-19 whose illness wasn't severe enough for them to be hospitalized, new research shows.
The American Psychological Association reports that researchers are scrambling to understand just how COVID-19 impacts the brain. Scientists are working to see what can be done to prevent long-term damage.
The prevalence of neurological problems remains an open question, but it’s safe to conclude that “neurological problems are not rare for COVID-19 patients,” says Majid Fotuhi, MD, PhD, medical director of NeuroGrow Brain Fitness Center and lead author of a comprehensive review of COVID-19’s effects on the nervous system (Journal of Alzheimer’s Disease, Vol. 76, No. 1, 2020). “Our best estimate so far is that 30% to 50% of hospitalized patients have neurological issues,”
Yale School of Medicine reported on February 15, 2021 that researches have connected spinal fluid autoantibodies to neurological symptoms of COVID-19 patients. Shelli Farhadian, MD, PhD, states “We found that most of the patients we studied had autoantibodies, or antibodies that target brain tissue, circulating in the spinal fluid. In one case, we found that antibodies that are directed against the virus were also cross-reacting against the brain. We think this might prove to be a link between the virus and the high rates of neurological symptoms that people show during and after COVID-19.”
Non‐hospitalized Covid‐19 “long haulers” experience prominent and persistent “brain fog” and fatigue that affect their cognition and quality of life, according to a recent March 23, 2021 article published by the Annals of Clinical and Translational Neurology.
Brain fog isn’t the only problem
"We found that fatigue, ill-health and breathlessness were all common following COVID-19," said Dr. Townsend of the Department of Infectious Diseases, St. James's Hospital and Department of Clinical Medicine, Trinity Translational Medicine Institute, Trinity College, Dublin, Ireland. "However, these symptoms appeared to be unrelated to the severity of initial infection or any single measurement at the time of an outpatient appointment."
Even people who are not hospitalized and who have mild illness can experience persistent or late long hauler symptoms. More studies are being conducted now due to the higher number of long-term complaints after COVID. The most commonly reported long-term symptoms include:
- Fatigue
- Shortness of breath
- Cough
- Joint pain
- Chest pain
Other reported long-term symptoms include:
- Difficulty with thinking and concentration "brain fog"
- Depression
- Muscle pain
- Headache
- Intermittent fever
- Fast-beating or pounding heart (also known as heart palpitations)
More serious long-term complications appear to be less common but have been reported. These have been noted to affect different organ systems in the body. These include:
- Cardiovascular: inflammation of the heart muscle
- Respiratory: lung function abnormalities
- Renal: acute kidney injury
- Dermatologic: rash, hair loss
- Neurological: smell and taste problems, sleep issues, difficulty with concentration, memory problems
- Psychiatric: depression, anxiety, changes in mood
Conclusion
As the COVID-19 spread begins to subside, are we entering a new health care crisis? As more health care workers contract even mild cases of COVID-19, will we continue to have a reduced professional health care workforce due to the long-term effects of COVID-19?
You are an important part of the health care workforce, whether you are a medical professional, coder, biller HIPAA officer, part of the C-Suite team or administration. Please, carefully consider all the possible short- and long-term side effects of getting or not getting the vaccine. Consult with your personal physician and dive into more resent research to find out more about the long-term affects you may experience if you should become a COVID-19 statistic.
Stay abreast of coding and documentation changes, consider our 2021 Diagnosis Coding Updates On-Demand Webinar and check out the Clinical Documentation Improvement course for medical practices, with the option to certify.
References
Annals of Clinical and Translational Neurology / March 23, 2021
American Psychological Association / November 1, 2020
CDC: Long-Term Effects of COVID-19 / November 13, 2020
Mayo Clinic / COVID-19 Long Term Effects / November 17, 2020
National Institutes of Health (NIH) / January 26, 2021
Yale School of Medicine / February 15, 2021